Cancer Sciences PhD/iPhD/MD/MSc (Research)
Our School of Cancer Sciences is a broad-based, research intensive institution with a global reach. We span fundamental cancer biology, translational and clinical cancer research. And focus on cancer genomics and disease-specific research. Our primary goal is to deliver world-class research that can be translated to patient benefit and to provide a leading-edge environment for research and training.
- PhD: 3-4 years full-time; 5 years part-time;
- IPhD: 5 years full-time;
- MSc (Research): 1 year full-time; 2 years part-time;
Research projects
All self-funded projects can be applied to throughout the year. Please note that not all projects are available in the IPhD route.
+++
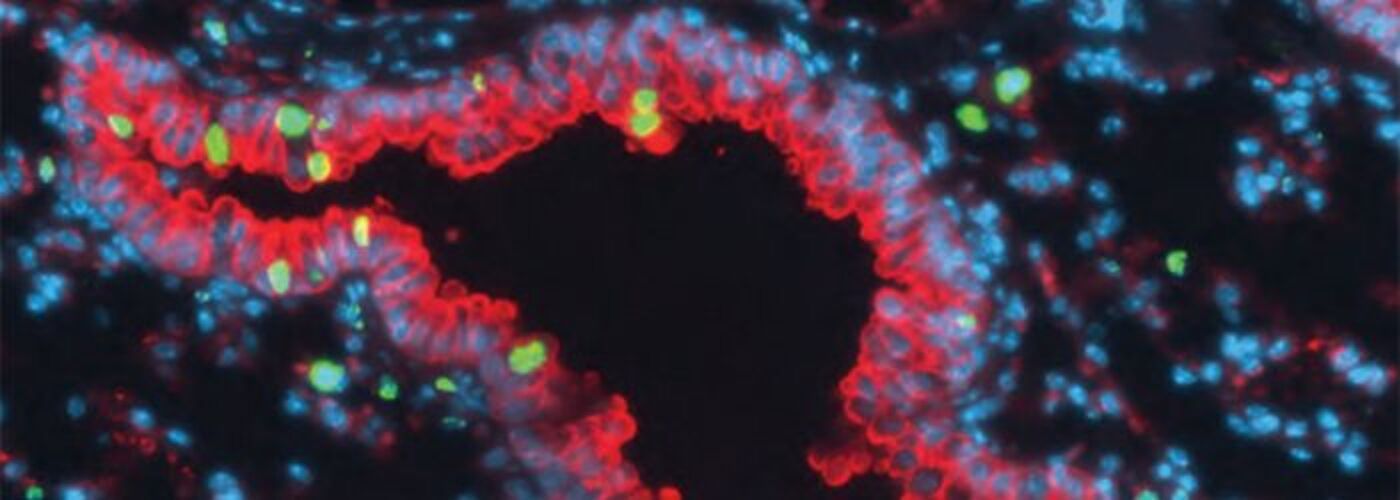
Investigating the Colonic Microbiome – Immune Interactions to Prevent Colorectal Cancer
Supervisors: Dr Stephen McSorley and Dr Johan Vande Voorde
Project description: Around 40% of individuals undergoing bowel screening colonoscopy have pre-malignant colorectal adenomas. Despite excising them patients remain at increased risk of further adenomas and colorectal cancer (CRC) in the future with no means of prevention available other than repeated colonoscopies.
Immune responses and infiltrates of specific subtypes of immune cells called T lymphocytes within adenomas are associated with a patient’s likelihood of future adenomas and CRC. It is unclear what drives differences in these immune responses to adenomas in the colon and ultimately outcomes.
The colonic microbiome – the variety and location of different species of bacteria, fungi and viruses within the large bowel - has been implicated in colorectal carcinogenesis including the formation of new adenomas and progression of adenomas to cancer. Furthermore, in established CRC, interaction between the microbiome and immune system is thought to impact outcomes.
This exciting PhD project will build on an existing highly annotated dataset of around 2600 patients who have undergone surveillance following polypectomy at bowel screening colonoscopy with matched tissue. The student will be involved in the prospective collection of colonic tissue and samples from patients having adenomas removed at colonoscopy. They will interrogate immune – microbiome interactions within adenoma and surrounding colonic biopsy tissue using techniques including immunohistochemistry, RNAseq, RNAscope, and state of the art spatial proteomic/transcriptomic technologies – Nanostring, GeoMx, DSP, and CosMx SMI.
The identification of specific immune system and microbiome targets associated with future adenoma risk will eventually permit drug screening and chemoprevention in a large group of high-risk patients for whom repeated colonoscopy is the only current management option.
Fees: There are no funds available for this PGR project. Applicants must have sufficient funds to pay for their support and PGR fees.
To apply, please contact supervisors and include project title in application.
---
Integrated PhD (October-April)
Our Integrated PhD combines an MSc and PhD project in a 1+3+1 format. There are two options when choosing to apply for the IPhD and these are shown below. Please review how to apply section for more information.
Option A: Choose from the listed projects.
You can select from the listed projects below and choose your MSc from the options listed on that project.
+++
Investigating the prognostic value of spatial immunophenotypes in lung cancer (available as IPhD)
Supervisors: Xiao Fu, John Le Quesne
MSc choice: Cancer Research & Precision Oncology [MSc]
Project description: Tumour microenvironments (TMEs) profoundly influence cancer progression and shape the response to anti-cancer therapy. Recent advances in digital pathology and innovative data analytics including machine learning have enhanced our ability to identify clinically relevant spatial characteristics of TMEs [1]. In lung cancer, several deep learning studies using Haematoxylin and Eosin (H&E) images have demonstrated that the spatial organisation of stromal and immune cell populations within the TME are relevant to tumour evolution and patient survival outcomes [2-4].
This PhD project will seek to investigate the prognostic value of spatial immunophenotypes in lung cancer combining high-plex imaging, spatial data analysis, and machine learning. One arm of the project will seek to engineer diverse quantitative features (e.g., adapting concepts and metrics from network science [5] to characterise cellular graphs) of the spatial immunophenotypes that are mapped in high-plex immunofluorescence images and evaluate their prognostic values in lung cancer. The other arm of the project will seek to develop deep learning models (e.g., adapting methods in [6]) based on spatial cellular graphs constructed from these images to predict clinical outcomes.
The research will be carried out using two comprehensively annotated cohorts of non-small-cell lung cancer patients, including LATTICe-A cohort (Leicester Archival Thoracic Tumour Investigatory Cohort- Adenocarcinoma), which comprises 1000 resected primary lung adenocarcinomas, and the Glasgow early non-small cell lung cancer cohort, which will comprise 1000 cases (including squamous cell carcinoma and other non-small cell varieties of lung cancer) upon completion next year. Several high-plex imaging methods (e.g., Vectra Polaris, PhenoCycler) will be applied to map spatial immunophenotypes, which are in addition to abundant genomic and RNA sequencing data as well as H&E images of the same tumours.
This project will be jointly supervised by Xiao Fu and John Le Quesne. The student will have an exciting opportunity to receive training in state-of-the-art imaging techniques, quantitative data analysis, and machine learning. The successful candidate will join the dynamic and collaborative research environment of the CRUK Beatson Institute, working with a diverse multidisciplinary team of computer scientists, bioinformaticians, clinicians, and experimental scientists.
References
- Fu X, Sahai E, Wilkins A. Application of digital pathology-based advanced analytics of tumour microenvironment organisation to predict prognosis and therapeutic response. J Pathol. 2023;260(5):578-591. doi:10.1002/path.6153
- AbdulJabbar K, Raza SEA, Rosenthal R, et al. Geospatial immune variability illuminates differential evolution of lung adenocarcinoma. Nat Med. 2020;26(7):1054-1062. doi:10.1038/s41591-020-0900-x
- Zhang H, AbdulJabbar K, Moore DA, et al. Spatial Positioning of Immune Hotspots Reflects the Interplay between B and T Cells in Lung Squamous Cell Carcinoma. Cancer Res. 2023;83(9):1410-1425. doi:10.1158/0008-5472.CAN-22-2589
- Quiros AC, Coudray N, Yeaton A, et al. Mapping the landscape of histomorphological cancer phenotypes using self-supervised learning on unlabeled, unannotated pathology slides. arXiv. 2023
- Albert-László Barabási. Network Science. Cambridge University Press. 2016. http://networksciencebook.com/
- Wu Z, Trevino AE, Wu E, et al. Graph deep learning for the characterization of tumour microenvironments from spatial protein profiles in tissue specimens. Nat Biomed Eng. 2022;6(12):1435-1448. doi:10.1038/s41551-022-00951-w
---
+++
Investigating the role of autophagy and mitochondrial function in leukaemic stem cells (available as IPhD)
Supervisors: Vignir Helgason, Eric Kalkman
MSc choice: Cancer Research & Precision Oncology [MSc]
Our lab is interested in biological processes that contribute to drug resistance in myeloid leukaemias, with particular focus on leukaemic stem cells (LSCs).
Introduction: Chronic myeloid leukaemia (CML) is caused by a reciprocal chromosomal translocation within a haemopoietic stem cell. This leads to transcription of BCR-ABL, a constitutively active tyrosine kinase that is necessary to induce CML.
The development of the tyrosine kinase inhibitor (TKI) significantly improved the life expectancy of CML patients; however, we have shown that disease persistence is caused by the remarkable ability of CML LSCs to survive, despite complete BCR-ABL inhibition mediated by TKI treatment1,2. Acute myeloid leukaemia (AML) is a more heterogeneous, involving different disease-causing genetic mutations. First line treatment for AML patients consists of chemotherapy, aiming at inducing remission. Generally, five-year survival rate in AML remains at a dismal 20%.
Activating internal tandem duplication mutations in FLT3 (FLT3-ITD), detected in about 20% of AML, represents driver mutations and a valid therapeutic target in AMLFLT-ITD. However, although new FLT3 inhibitors have begun to show promising clinical activity it is unlikely that they will have durable effects as single agents In recent years there has been resurgence in interest in autophagy, energy metabolism and mitochondria function as a possible area for development of novel anti-cancer agents.
We recently developed improved protocols for autophagy and metabolic assays in rare LSCs and highlighted mitochondrial oxidative phosphorylation (OXPHOS) as a metabolic dependency in CML LSCs3. Primitive AML cells have also been shown to depend on increased mitochondrial respiration4,5. We will therefore further investigate mitochondrial metabolism and through validation of drug-repurposing screen, identify new clinically applicable drugs that inhibit OXPHOS in CML, and in AML where improved therapy options with acceptable toxicities are urgently needed.
Hypothesis/aims: Our working hypothesis is that autophagy and deregulated mitochondrial metabolism in LSCs renders them sensitive to inhibition of the ULK1 autophagy complex and pathways that sustain mitochondrial OXPHOS. Our first aim is to use complementary functional and omic approaches to further assess the dependency of CML/AML LSCs to recycle or oxidise major mitochondrial fuels (objective 1). Our second aim is to test ULK1 inhibitors6 and FDA-approved OXPHOS inhibitors (which we have recently identified through drug-repurposing screening), in combination with TKI treatment, for eradication of CML and AMLFLT3-ITD/TKD LSCs (objective 2).
Deliverables: This project will therefore promote identification of a core fuel pathway signature of CML/AML LSCs and a set of new potentially selective LSC-specific metabolic drug targets (objective 1). The student will also use state-of-the-art in vitro and in vivo models to test clinically relevant drugs, which will in the longer term, facilitate the translation of our findings into the clinic, with the overall aim for CML and AML LSC eradication.
References
- Holyoake, T.L., et al. Immunological reviews. 106-23 (2015).
- Hamilton, A., et al. Blood. 1501-10 (2012).
- Kuntz, E.M., et al. Nat Med. 1234-40 (2017).
- Skrtic, M., et al. Cancer Cell. 674-88 (2011).
- Lagadinou, E.D., et al. Cell Stem Cell. 329-41 (2013).
- Ianniciello, A., et al. Sci Transl Med. (2021)
---
+++
Microenvironment in paediatric and adult acute myeloid leukaemia (available as IPhD)
Supervisor: Dr Karen Keeshan
MSc choice: Cancer Research & Precision Oncology [MSc]
Abstract: Acute myeloid leukaemia (AML) is a genetically and phenotypically heterogeneous disease that is characterized by a block in myeloid differentiation, as well as enhanced proliferation and survival. It affects people of all ages with an incidence of 2-3 per 100 000 per annum in children, increasing to 15 per 100 000 per annum in older adults. The relapse risk for childhood AML remains unacceptably high and relapse is the commonest cause of death. Multiple courses of chemotherapy remain the mainstay of treatment in adult and childhood AML but a ceiling of benefit has been reached and toxicity is significant (Chaudhury et al, 2015). There have been few, if any, new treatments in the past 30 years and there is a pressing need for novel effective therapies in AML.
The treatment of paediatric AML is in essence extrapolated from that of adults with AML. Our previous work (Chaudhury et al, 2018) have questioned the appropriateness of this approach which assumes that a similar aetiology underlies AML in the young and old, . providing evidence that disease characteristics differ between a paediatric and adult population with AML Functional interplay between AML cells and the bone marrow microenvironment is a distinctive characteristic of AML disease. AML cells in the adult bone marrow BM reside in leukaemic niches (Aung et al. 2020) that support leukaemic cell survival and expansion. The importance of the microenvironment in paediatric versus adult AML (fetal liver, cord blood, bone marrow) and its role is disease characteristics has not been well explored. Our lab focuses on the proliferation and self-renewal capabilities of the leukaemic cell and the influence of the leukaemic niche including mesenchymal stem cells. We hypothesize that the microenvironment influences the initiation, maintenance, and aggressiveness of paediatric and adult AML disease.
Methods & approaches: This project will investigate the role of the microenvironment in AML disease initiation and maintenance,. particularly the crosstalk between mesenchymal stem cells and AML cells and how it impacts disease chemoresistance and relapse.
We will focus on genetically distinct subtypes of paediatric and adult using a number of models and approaches including: Bone marrow transduction and transplantation (BMT) murine models: expression of AML oncogenes in viral constructs and using CRISPR/Cas9 gene editing approaches; assessments on disease in vivo; Stromal co-cultures and transcriptional profiling using single cell RNA-sequencing; primary AML samples from paediatric and adult patients. The project will also employ flow cytometry, cellular and molecular biology technologies. This PhD studentship offers extensive dual training in both fundamental and translational biology of leukaemia, an environment encompassing clinical and basic researchers, and training opportunities as part of the college graduate programme.
References
-
Chaudhury SS, Morison JK, Gibson BES, Keeshan K. Insights into cell ontogeny, age and acute myeloid leukaemia. Experimental Hematology. 2015 Jun 4.
-
Chaudhury S, O'Connor C, Canete A, Bittencourt-Silvestre J, Sarrou E, Prendergast A, Choi J, Johnston P, Wells CA, Gibson B, Keeshan K. Age-specific biological and molecular profiling distinguishes paediatric from adult acute myeloid leukaemias. Nat Commun. 2018;9(1):5280
-
Aung MMK, Mills ML, Bittencourt-Silvestre J, Keeshan K. Insights into the molecular profiles of adult and paediatric acute myeloid leukaemia. Mol Oncol. 2021;15(9):2253-72.
---
+++
Understanding and exploiting immunogenic cell death to treat cancer (available as IPhD)
Supervisors: Stephen Tait, Ed Roberts
MSc choice: Cancer Research & Precision Oncology [MSc]
Project description: Cell death both prevents and treats cancer. New anti-cancer therapies that directly target cell death are revolutionising the treatment of cancer. Nevertheless, a major problem to effective cancer treatment is the emergence of treatment resistance. We are interested in killing cancer cells in a way that alerts the immune system to the presence of cancer - in essence harnessing the power and adaptability of tumour immunity to eradicate cancer. Our focus is on mitochondrial apoptosis - we have found that blocking caspase protease activity makes cell death immunogenic.
This PhD project will seek to understand why such caspase-inhibited cell death is immunogenic - both at the level of the dying cell but also in understanding how the immune system responds to the dying cell. We will employ novel approaches to inhibit caspase activity. In short, this exciting project will focus on discovery science with clear translation impact for cancer treatment.
The techniques it will entail will be varied but include CRISPR-Cas9 genome editing, super-resolution microscopy and in vivo modelling of cancer. This will be a collaborative project jointly supervised by Stephen Tait and Ed Roberts. You will join a young, dynamic interdisciplinary research team, based withing the CR-UK Beatson Institute with access to cutting edge technology.
References
- Targeting immunogenic cell death in cancer. Ahmed A, Tait SWG. Mol Oncol. 2020 Dec;14(12):2994-3006. doi: 10.1002/1878-0261.12851. Epub 2020 Dec 1.
- Mitochondrial permeabilization engages NF-κB-dependent anti-tumour activity under caspase deficiency
---
Option B: Create your own research proposal
You can create your own project, source a supervisor and they will choose an MSc programme that aligns with your research proposal.
+++
Create your own PhD proposal
- Create your own proposal - approximately 1000 words and must include:
- a straightforward, descriptive, and informative title
- the question that your research will address
- an account of why this question is important and worth investigating
- an assessment of how your own research will engage with recent research in the field
- a brief account of the methodology and approach you will take.
- You will need to contact a supervisor prior to application, using the search function.
Based on your proposal, your supervisor will choose an MSc programme that aligns with your research interests.
---
Overview
We are part of a national centre of excellence in the fight against cancer carrying out a programme of world-class science directed at understanding the molecular changes that cause cancer. We are working to translate scientific discoveries into new drugs or diagnostic and prognostic tools that benefit cancer patients, taking new therapies through preclinical and clinical trials.
The School of Cancer Sciences is a major component of the Cancer Research UK West of Scotland Cancer Centre. There are currently 51 research groups housed in magnificent new research buildings at the Beatson Institute for Cancer Research, the Paul O’Gorman Leukaemia Research Centre, the CRUK clinical trials unit (CTU) and the Wolfson Wohl Cancer Research Centre. Our facilities house a number of state-of-the-art technologies that underpin our key research themes.
Individual research projects are tailored around the expertise of principal investigators within our Schools. Basic and clinical projects are also available for study.
A variety of approaches are used, including molecular biology, biochemistry, bioinformatics, genetics, cancer modelling and cell biology (including advanced in vitro and in vivo imaging), immunology and polyomics (genomics, transcriptomics, proteomics and metabolomics).
Specific areas of interest include:
- cancer biology and cell signalling
- epigenetics
- cancer stem cell biology
- cancer imaging
- chemoresistance in cancer
- cancer and ageing
- regulation of cancer cell death processes
- genetics, genomics and systems medicine
- immunotherapy for cancer
- cancer clinical trials
Study options
PhD
- Duration: 3/4 years full-time; 5 years part-time
Individual research projects are tailored around the expertise of principal investigators.
Integrated PhD programmes (5 years)
Our Integrated PhD allows you to combine masters level teaching with your chosen research direction in a 1+3+1 format.
International students with MSc and PhD scholarships/funding do not have to apply for 2 visas or exit and re-enter the country between programmes. International and UK/EU students may apply.
Year 1
Taught masters level modules are taken alongside students on our masters programmes. Our research-led teaching supports you to fine tune your research ideas and discuss these with potential PhD supervisors. You will gain a valuable introduction to academic topics, research methods, laboratory skills and the critical evaluation of research data. Your grades must meet our requirements in order to gain entry on to your pre-selected PhD research project. If not, you will have the options to pay outstanding MSc fees and complete with masters degree only.
Years 2, 3 and 4
PhD programme with research/lab work, completing an examinable piece of independent research in year 4.
Year 5
Thesis write up.
MSc (Research)
- Duration: 1 year full-time; 2 years part-time
MD (Doctor of Medicine)
- Duration: 2 years full-time; 4 years part-time (for medically-qualified graduates only)
Entry requirements
A 2.1 Honours degree or equivalent.
English language requirements
For applicants from non-English speaking countries, as defined by the UK Government, the University sets a minimum English Language proficiency level.
International English Language Testing System (IELTS) Academic and Academic Online (not General Training)
- 6.5 with no subtests under 6.0
- IELTS One Skill Retake Accepted
- Tests must have been taken within 2 years 5 months of start date. Applicants must meet the overall and subtest requirements using a single test.
Common equivalent English language qualifications for entry to this programme
TOEFL (ibt, mybest or athome)
- 90 overall with Reading 20; Listening 19; Speaking 19; Writing 21
- Tests must have been taken within 2 years 5 months of start date. Applicants must meet the overall and subtest requirements, this includes TOEFL mybest.
Pearsons PTE Academic
- 59 with minimum 59 in all subtests
- Tests must have been taken within 2 years 5 months of start date. Applicants must meet the overall and subtest requirements using a single test.
Cambridge Proficiency in English (CPE) and Cambridge Advanced English (CAE)
- 176 overall, no subtest less than 169
- Tests must have been taken within 2 years 5 months of start date. Applicants must meet the overall and subtest requirements using a single test.
Oxford English Test
- 7 overall with no subtest less than 6
- Tests must have been taken within 2 years 5 months of start date. Applicants must meet the overall and subtest requirements using a single test.
LanguageCert Academic SELT
- 70 overall with no subtest less than 60
- Tests must have been taken within 2 years 5 months of start date. Applicants must meet the overall and subtest requirements using a single test.
Password Skills Plus
- 6.5 overall with no subtest less than 6.0
- Tests must have been taken within 2 years 5 months of start date. Applicants must meet the overall and subtest requirements using a single test.
Trinity College Tests
- Integrated Skills in English II & III & IV: ISEII Distinction with Distinction in all sub-tests
- Tests must have been taken within 2 years 5 months of start date. Applicants must meet the overall and subtest requirements using a single test.
University of Glasgow Pre-sessional courses
- Tests are accepted for 2 years following date of successful completion.
Alternatives to English Language qualification
- Degree from majority-English speaking country (as defined by the UKVI including Canada if taught in English)
- students must have studied for a minimum of 2 years at Undergraduate level, or 9 months at Master's level, and must have completed their degree in that majority-English speaking country within the last 6 years.
- Undergraduate 2+2 degrees from majority-English speaking country (as defined by the UKVI including Canada if taught in English)
- students must have completed their final two years study in that majority-English speaking country within the last 6 years.
For international students, the Home Office has confirmed that the University can choose to use these tests to make its own assessment of English language ability for visa applications to degree level programmes. The University is also able to accept UKVI approved Secure English Language Tests (SELT) but we do not require a specific UKVI SELT for degree level programmes. We therefore still accept any of the English tests listed for admission to this programme.
Pre-sessional courses
The University of Glasgow accepts evidence of the required language level from the English for Academic Study Unit Pre-sessional courses. We would strongly encourage you to consider the pre-sessional courses at the University of Glasgow's English for Academic Study (EAS) Unit. Our Pre-sessional courses are the best way to bring your English up to entry level for University study. Our courses give you:
- direct entry to your University programme for successful students (no need to take IELTS)
- essential academic skills to help you study effectively at University
- flexible entry dates so you can join the right course for your level.
For more detail on our pre-sessional courses please see:
We can also consider the pre-sessional courses accredited by the below BALEAP approved institutions to meet the language requirements for admission to our postgraduate taught degrees:
- Heriot Watt
- Kingston Upon Thames
- Middlesex University
- Manchester University
- Reading University
- Edinburgh University
- ST Andrews University
- UCL
- Durham.
Fees and funding
Fees
2025/26
- UK: £5,005
- International & EU: £31,800
Prices are based on the annual fee for full-time study. Fees for part-time study are half the full-time fee.
Irish nationals who are living in the Common Travel Area of the UK, EU nationals with settled or pre-settled status, and Internationals with Indefinite Leave to remain status can also qualify for home fee status.
Alumni discount
We offer a 20% discount to our alumni on all Postgraduate Research and full Postgraduate Taught Masters programmes. This includes University of Glasgow graduates and those who have completed Junior Year Abroad, Exchange programme or International Summer School with us. The discount is applied at registration for students who are not in receipt of another discount or scholarship funded by the University. No additional application is required.
Possible additional fees
- Re-submission by a research student £540
- Submission for a higher degree by published work £1,355
- Submission of thesis after deadline lapsed £350
- Submission by staff in receipt of staff scholarship £790
Depending on the nature of the research project, some students will be expected to pay a bench fee (also known as research support costs) to cover additional costs. The exact amount will be provided in the offer letter.
Funding
The IPhD is not supported by University of Glasgow Scholarship/Funding
- Recruitment at the Beatson Institute (postdoctoral/clinical research fellowships and PhD studentships)
- BBSRC Doctoral Training Partnerships
- External funding information
Support
The College of Medical, Veterinary and Life Sciences Graduate School provides a vibrant, supportive and stimulating environment for all our postgraduate students. We aim to provide excellent support for our postgraduates through dedicated postgraduate convenors, highly trained supervisors and pastoral support for each student.
Our overarching aim is to provide a research training environment that includes:
- provision of excellent facilities and cutting edge techniques
- training in essential research and generic skills
- excellence in supervision and mentoring
- interactive discussion groups and seminars
- an atmosphere that fosters critical cultural policy and research analysis
- synergy between research groups and areas
- extensive multidisciplinary and collaborative research
- extensive external collaborations both within and beyond the UK
- a robust generic skills programme including opportunities in social and commercial training
How to apply
Identify potential supervisors
All postgraduate research students are allocated a supervisor who will act as the main source of academic support and research mentoring. You must identify a potential supervisor and contact them to discuss your research proposal before you apply. Please note, even if you have spoken to an academic staff member about your proposal you still need to submit an online application form.
IPhD & research projects
IPhD Option A
Applicants do not need to contact a supervisor. You will choose from a list of IPhD projects and each project has named supervisors linked to that project.
IPhD Option B
You will submit a research proposal of approximately 1000 words. The proposal must include:
- a straightforward, descriptive, and informative title
- the question that your research will address
- an account of why this question is important and worth investigating
- an assessment of how your own research will engage with recent research in the field
- a brief account of the methodology and approach you will take.
Based on your proposal, your supervisor will choose an MSc programme that aligns with your research interests.
You will need to contact a supervisor prior to application, using our search to identify a suitable supervisor.
Research projects
If you are seeking to apply for any research project, you can identify this within your application to the PhD programme. Please ensure that you highlight the title of the research project you are interested in on your application.
Gather your documents
Before applying please make sure you gather the following supporting documentation:
- Final or current degree transcripts including grades (and an official translation, if needed) – scanned copy in colour of the original document.
- Degree certificates (and an official translation, if needed): scanned copy in colour of the original document.
- Two references on headed paper and signed by the referee. One must be academic, the other can be academic or professional (except IPhD applicants, where only one academic or professional reference is required). References may be uploaded as part of the application form or you may enter your referees' contact details on the application form. We will then email your referee and notify you when we receive the reference.
- Research proposal (if applying for PhD or MScR), CV, samples of written work as per requirements for each subject area.
Contact us
If you require assistance before you apply: mvls-gradschool@glasgow.ac.uk
After you have submitted your application: Admissions Enquiries form
Our research environment
Induction
- Getting started with PGR development: how postgraduate researchers are welcomed into our community

