Engineering better outcomes for drug discovery
Glasgow bioengineers are applying their understanding of the way our cells function and grow to improve the process of discovering new medicines.
The scientists from Glasgow’s Centre for the Cellular Microenvironment, led by Professor Manuel Salmeron-Sanchez and Professor Matthew Dalby, develop novel techniques and materials to direct and control the behaviour of cells.
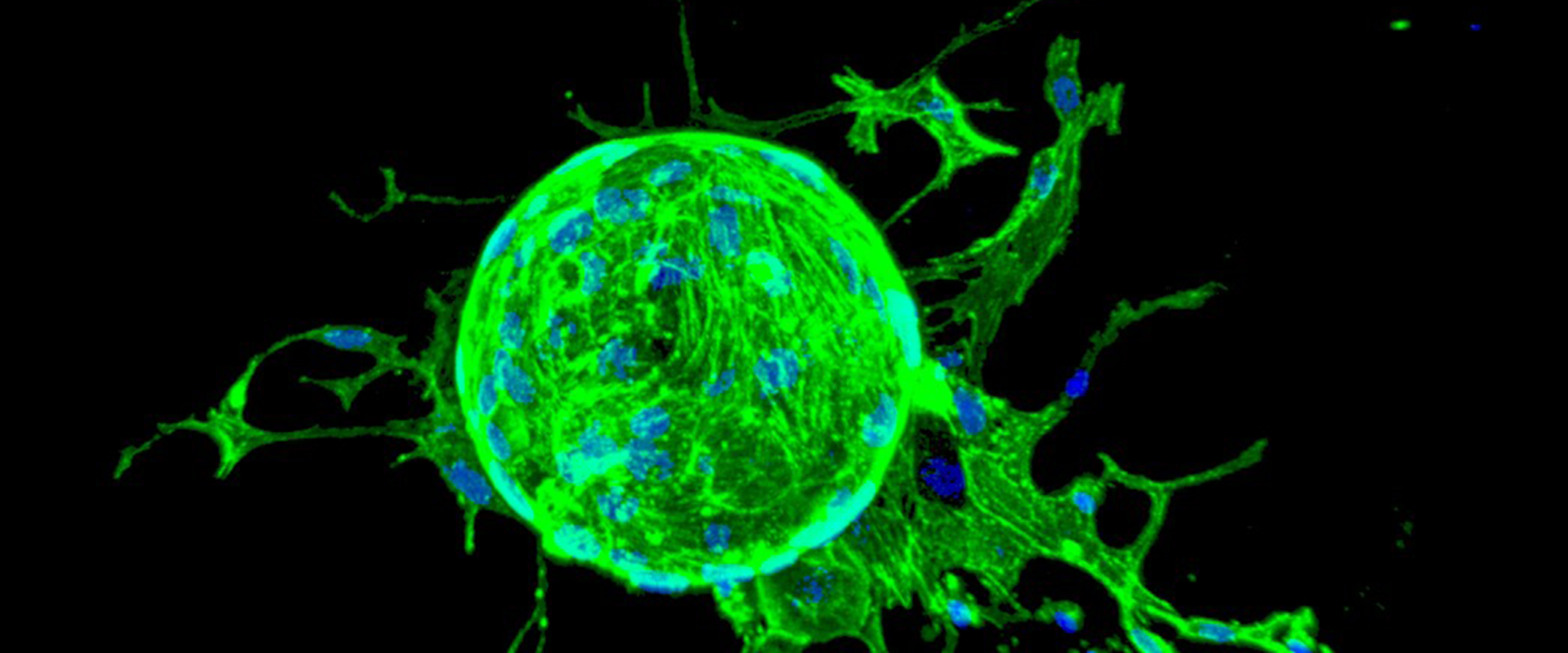
One aim of this work is develop better in vitro (lab-based) models for drug screening. This involves using cell engineering techniques to grow small tissue samples in the lab that model organs and systems within the body (organoids). This is the field of non-animal technologies.
In a major boost for this research, Glasgow is leading on a new Centre for Doctoral Training. Each year, the lifETIME (Engineered Tissues for Discovery, Industry and Medicine) CDT will train a cohort of PhD students to become specialists this field.
Addressing the productivity problem for pharmaceuticals
Advances in research and development for developing pharmaceuticals have meant there are huge numbers of molecules created that can potentially become medicines. The problem is that too many make it through initial screening only to fail later when the clinical trial costs are much higher.
The researchers in the Centre for the Cellular Microenvironment hope non-animal technologies will create better cell culture systems for these screens, as they will more accurately reflect the behaviour of cells and the cell environment within the human body.
Professor Dalby explains how their research can have an impact on the development of new medicines.
“In their trials, the pharmaceutical industry have typically used a very simplistic cell screen in the first instance. They follow this with animal testing to weed out further false hits.”
“These techniques miss many false positives before they move into expensive clinical trials. 43% of false positives still make it into the first human trials.”
“These poor outcomes arise from the fact that animal models or cells growing in a petri dish do not accurately represent human conditions.”
“The CDT and a lot of our work will focus on developing humanised 3D organoids, tissues, microfluidic systems, sensing and detection systems from which to put together non-animal technologies for drug screening. These will predict drug fails earlier and provide better leads to take through to human trials.”
Progress in this field should reduce the cost of drug trials and increase productivity, as molecules with no drug potential are eliminated earlier, thereby giving focus to those with better prospects. With less money spent on failed clinical trials, it should also reduce the overall cost of drugs.
In one example of their work, Professor Manuel Salmeron-Sanchez, describes how drugs developed to target the brain often fail at the human trial stage.
“When a drug has been designed, it is hard to determine if it will cross the blood brain barrier or not. The trials to test these drugs use animal models but these are not representative of the human blood brain barrier. We hope to develop a robust model in vitro that can predict if a drug will be able to cross the blood brain barrier in humans or not.”
Potential for personalised medicine
Professor Salmeron-Sanchez also describes how these non-animal technologies could also have an important role in the future for personalised medicine. In this scenario, drug screening goes beyond testing for use in the general population and the focus switches to an individual’s response – or lack of – to a certain type of treatment.
“These organoids can be made using cells from the patient that is going to receive a drug treatment, for example in cancer treatments. Using cells from the patient that have been grown to form an organoid, the dosage and the possible patient response can be better analysed before they start the treatment.”
To enable it to work towards these objectives, the lifETIME CDT has close partnerships with the pharmaceutical industry, the NHS, regulatory bodies and leading charities.
Glasgow’s university partners for the CDT are Birmingham, Aston and Galway. Each brings a unique specialisation to the development of regenerative medicine and non-animal technologies. Students are able to base themselves at any one of the four universities to complete their PhD.
The Centre for the Cellular Microenvironment
The Centre for the Cellular Microenvironment was established in 2018 to consolidate important research relationships that already existed across the University structure.
Their next step is to move into Glasgow’s new £113 million research hub. This will bring the researchers of the Centre properly together for the first time, enabling them to develop on one site.
“Moving into the Research Hub is a great opportunity to have shared space and shared labs. Our ultimate ambition is to have an institute focused on microenvironments, with research that can be applied to areas like regenerative medicine and non-animal technologies” says Professor Salmeron-Sanchez.
“In this field, we need biologists, we need engineers, we need chemists and we need physicists for it all to work.”
With important connections to the Veterinary School and Medical School, Glasgow provides an excellent environment for not only their fundamental research but also the translational work - taking things through to treatments for animals and humans. The Centre also relies heavily on the data collection and analysis of Glasgow Polyomics.
“We are broad enough to cover the full spectrum of work. We can develop our own fundamental research and ideas, but we can then move these through the innovation stage to real clinical trials.” says Professor Salmeron-Sanchez.
By pulling all of these capabilities together, and establishing a new base of talent with the lifETIME CDT, Professor Dalby hopes the Centre will build a global reputation for excellence in regenerative medicine and its related fields.
“We want to use this coming together as a way to enhance our reputation internationally. We want the Centre to be a real beacon of world-class biomedical materials research in the UK, in Europe and across the world. With this critical mass of personnel and research, we can attract even more really great talent.”
For more information on the Centre’s work on regenerative medicine, see: Breakthroughs in Bone Regeneration.

